Hypnosis for Smoking Cessation
Amelia Amen
Efforts to quit smoking can be a challenging process for individuals who have developed a dependency on nicotine. When an individual tries to remove smoking from their daily routine, they may be prone to experiencing withdrawals. Such withdrawals include irritability, headaches, difficulty concentrating, and a strong craving for nicotine. According to the Centers for Disease Control and Prevention, smoking is one of the leading preventable causes of death in the U.S and often causes diseases such as lung cancer, heart disease, diabetes, and more.
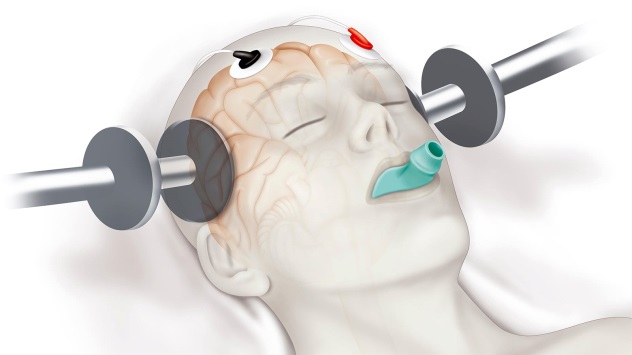
Hypnosis has been found to be a successful technique which aids in smoking cessation and other harmful behaviors. Hypnosis focuses on reducing and changing negative habits and developing self-control over certain emotions and behavior. It can be a source of treatment for helping the smoker remove many unwanted behaviors and habits. In the case of nicotine addiction, hypnosis is used to diminish the craving within the mind. Hypnosis targets the parts of our minds that can be the root cause of the motivation to smoke. The desire to smoke is often triggered by stress and anxiety, finishing a meal, going to a social event, driving, boredom, and more. Hypnosis is a collaborative process between the therapist and patient. Hypnosis only works when the patient wants to learn it. Eventually, the therapist teaches the patient how to achieve a state of hypnosis so they will be able to substitute positive messages for the prior negative ones which will help achieve their goal to stop smoking.
When a therapist performs hypnosis, he or she will guide the individual into a meditative state. Within this state of mind, the therapist may compare the odor of cigarette smoke to an unpleasant one such as truck exhaust. Another suggestion a therapist may make is that smoking will do nothing but poison your body, and how you should protect your body from such poisons. Our methods were taught to us by Dr. Herbert Spiegel of Columbia University, he is well known for his smoking cessation hypnosis technique. One of the goals of hypnosis is to help the patient become receptive of new ideas and thoughts about smoking. Although hypnosis is an effective way to aid smoking cessation, it is important to keep in mind that it will be most effective with continuous sessions along with the commitment of quitting.
If you or someone you know is seeking hypnosis to stop smoking or other negative behaviors that are troubling you, please contact our psychotherapy offices in New York or New Jersey to talk to one of our licensed professional psychologists, psychiatrists, psychiatric nurse practitioners, or psychotherapists at Arista Psychotherapy & Psychiatric Services. Contact our Manhattan, NY or Paramus, NJ offices respectively at (201) 368-3700 or (212) 722-1920 to set up an appointment. For more information, please visit https://www.counselingpsychotherapynjny.com
Source: