Intergenerational Trauma: What is it?
By Erika Ortiz
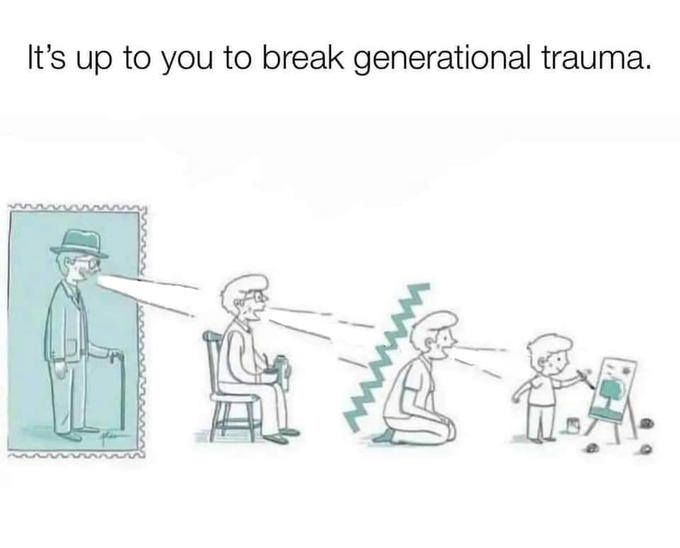
Intergenerational trauma is a term used to describe the difficulties or challenges a family has experienced for generations. Intergenerational trauma can inflict negative feelings and experiences through either an individual or the family as a whole. It usually starts with one family member who has had a traumatic experience. The family members then goes on to either repeat the action that traumatized them or project their feelings onto family members, continuing the cycle of trauma. Historical trauma can catalyze intergenerational trauma. For example, a great-grandmother survived the Holocaust; however, she now behaves in a very reserved and cold manner, so she struggles to express emotions such as love and compassion. Since she raised her children in such a manner, they may grow and have children and display that same type of avoidant relationship. Another example can be that a mother was sexually abused when she was younger, her daughter was also sexually abused, and her granddaughter suffered from that experience. The individual who suffers the trauma can pass down and then project the feelings that were felt at the time of the incident. Since they most likely did not receive the proper care and treatment to manage the mental health issues that they were experiencing, they relayed that same traumatic feeling to the next generation of their family. Hence, it is critical to seek professional help. Here are some ways to cope/deal with inter-generational trauma:
- Break the cycle- interrupt and prevent the repetition of trauma
- Hear each other out- although this can be difficult, listening is key to fixing
- Get the professionals involved- the best way to cope with any mental health issue or fragmented relationship is to get a qualified professional’s help
Source:
https://www.choosingtherapy.com/intergenerational-trauma/
If you or someone you know is experiencing intergenerational trauma or other traumas, please contact our psychotherapy offices in New York or New Jersey to talk to one of our licensed professional psychologists, psychiatrists, psychiatric nurse practitioners, or psychotherapists at Arista Counseling & Psychotherapy. Contact our Paramus, NJ or Manhattan, NY offices respectively at (201) 368-3700 or (212) 722-1920 to set up an appointment. For more information, please visit https://www.counselingpsychotherapynjny.com









