Social Media: The Impact on Mental Health
By: Maria Koutsothanasis
Social media plays a significant role in shaping how we connect, communicate, and even view ourselves. While social media has its benefits, it can also have a detrimental impact on mental health. Social media can negatively affect our mental well-being through constant comparisons, unrealistic expectations, and exposure to harmful content. By being intentional about what we engage with, we can use social media as a tool to enhance our lives and protect our mental well-being.
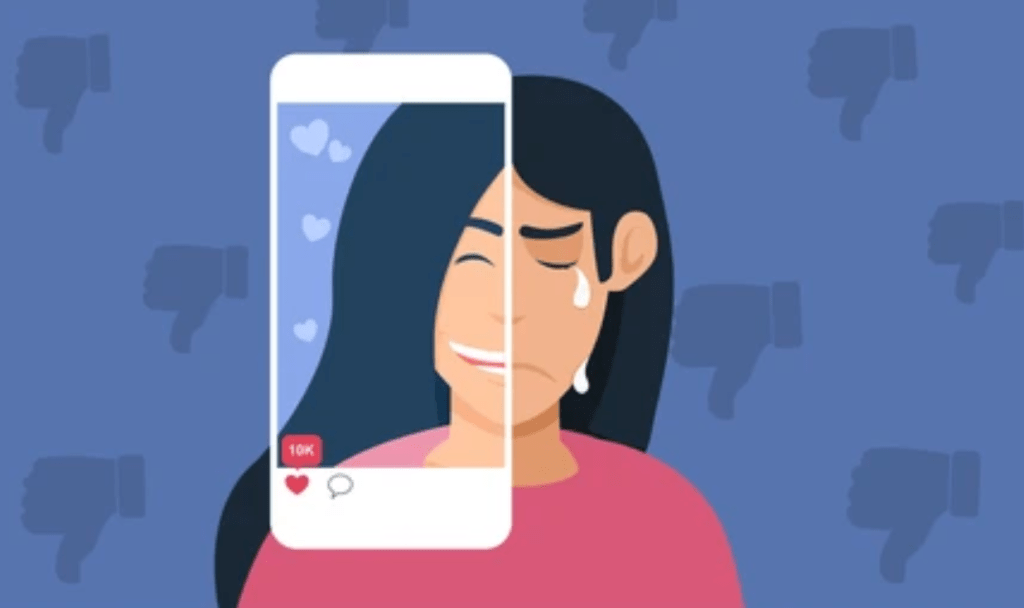
One of the main drawbacks of social media is the tendency to compare ourselves to others. Platforms such as Instagram and TikTok are often filled with images of people’s “perfect” lives, highlighting their achievements, beauty, and happiness. This can lead to feelings of inadequacy and low self-esteem, especially when we find ourselves measuring our lives against these unrealistic portrayals. Social media comparison can lead to symptoms of anxiety, depression, and even body image issues. The more we focus on the idealized versions of others’ lives, the more likely we are to forget that what we see online isn’t always an accurate reflection of reality.
The positive aspect is that we can decide what content we engage with. By intentionally following accounts that promote positivity, self-love, and well-being, we can counteract the negative effects. Following fitness influencers who focus on health rather than body perfection, or mental health advocates who offer advice and share stories of resilience, can create a more positive environment. By engaging with content that aligns with our values, we can shift our mindset toward growth and self-empowerment.
Social media often highlights negativity, which can significantly affect our mental well-being. Platforms frequently highlight drama, conflicts, and extreme opinions, contributing to constant criticism and judgment. Posts that focus on problems, such as failed relationships, mental health struggles, or societal issues, can evoke anxiety or feelings of hopelessness. Viral content that spreads negativity, such as gossip or inflammatory comments, often gains attention, while positive messages may not receive the same recognition. This constant exposure to pessimism can leave individuals feeling overwhelmed and disconnected from the positive aspects of life.
While social media has its negative aspects, it’s possible to transform how we interact with it to protect our mental health. By being mindful of the content we consume and consciously seeking out positive, uplifting posts, we can create an online environment that nurtures our well-being. Social media can be a powerful tool for connection, education, and personal growth if used intentionally. Ultimately, it is important to remember that we control our social media environment and can shape it to support our mental health.
If you or someone you love is struggling with depression or anxiety, please contact our psychotherapy offices in New York or New Jersey to talk to one of our licensed professional psychologists, psychiatrists, psychiatric nurse practitioners, or psychotherapists at Arista Counseling and Psychotherapy. Contact our Paramus, NJ or Manhattan, NY offices respectively, at (201) 368-3700 or (212) 722-1920 to set up an appointment. For more information, please visit http://www.counselingpsychotherapynjny.com/.
UC Davis Health. (2024, November 27). Social Media’s impact on our mental health and tips to use it safely. health. https://health.ucdavis.edu/blog/cultivating-health/social-medias-impact-our-mental-health-and-tips-to-use-it-safely/2024/05