By Danielle Mendler
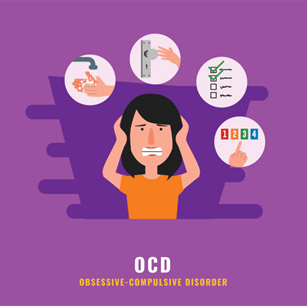
Obsessive-Compulsive Disorder is a disorder where obsessions lead to compulsive behavior. These obsessions take the form of intrusive thoughts that cause discomfort, anxiety, and stress. The compulsions that follow these thoughts are actions that people struggling with OCD take to relieve those intense unpleasant feelings.
A notorious OCD stereotype is washing hands. Someone with Obsessive Compulsive Disorder may get an intrusive thought into their head along the lines of “You haven’t been careful enough today. You have to wash your hands again because you didn’t do it right the first time. If you don’t you will get everyone you love sick because YOU weren’t careful.” These thoughts consume those with OCD and the victim will believe everything this voice is telling them. Therefore, to stop the anxiety and guilt, they will wash their hands over and over again until it feels right. This will repeat multiple times a day causing extreme stress on this person and getting in the way of their daily routine.
However, OCD isn’t always about staying clean or being organized. These obsessions can take the form of anything. This disorder attacks what the victim cares about most. An example is Scrupulosity. Scrupulosity is when people have intense OCD attacks on their religion and morals. This will happen when a person is extremely invested in their faith. The disorder overtakes what they enjoy and causes stress and chaos to it, making them feel like they will never be kind enough or religious enough. Some OCD takes the form of more irrational thoughts and actions that don’t always make sense to everyone else except them. People will believe that if they don’t knock on the floor four times, somebody they love will get hurt, just because their brain is telling them that. This obsessive thought causes enough internal conflict to result in the victim committing the compulsion of hitting the floor. It may seem harmless but these thoughts and actions over take people lives.
Obsessive Compulsive Disorder can create many obstacles in daily life. People with OCD have trouble showing up on time to school or work, because they compulsions made them late. They can be under a constant state of stress and can have panic attacks over triggering words/actions that may not have significance to anyone else. If their compulsive actions include any physical activity (scratching, washing, etc.) it can cause bodily harm.
Obsessive Compulsive Disorder is a very serious mental health crisis that affects people daily. If you or someone you know is struggling with OCD or any other stress please contact Arista Counseling and Psychological Services at 201-368-3700.